Caring for someone with mobility challenges means thinking beyond basic needs. Mealtime becomes more complex when your loved one has stroke effects, Parkinson’s disease, or other disabilities.
This caregiver’s guide to adaptive dining will help you create better eating experiences. It’s not just about having the right tools. Success comes from understanding the whole dining environment.
Many families focus only on buying special equipment. However, the best results happen when you combine good tools with smart techniques.
Your role as a caregiver extends beyond serving food. You become a dining coach, environmental designer, and support system all at once.
This guide covers everything you need to know. We’ll explore how to set up spaces, assist with feeding, and maintain dignity during meals.
Whether you’re caring for someone with recent changes or long-term conditions, these strategies will help both of you feel more confident at mealtime.
- UNDERSTANDING YOUR ROLE IN ADAPTIVE DINING
- ASSESSING INDIVIDUAL DINING NEEDS
- CREATING THE PERFECT DINING ENVIRONMENT
- SMART MEAL PREPARATION STRATEGIES
- FEEDING ASSISTANCE TECHNIQUES
- MANAGING COMPLEX CONDITIONS
- SUPPORTING INDEPENDENCE AND DIGNITY
- FAMILY AND SOCIAL DINING
- TECHNOLOGY AND MODERN SOLUTIONS
- NUTRITIONAL MONITORING AND HEALTH
- CAREGIVER SELF-CARE AND SUPPORT
- LONG-TERM PLANNING AND EQUIPMENT CHANGES
- CONCLUSION
UNDERSTANDING YOUR ROLE IN ADAPTIVE DINING
As a caregiver, you wear many hats during mealtime. First, you’re an observer who watches for changes in eating abilities.
Next, you become a problem-solver when challenges arise. Most importantly, you’re a supporter who helps maintain independence.

Your job isn’t to take over completely. Instead, you help your loved one do as much as possible on their own.
This approach keeps their skills sharp and protects their self-esteem. It also makes your job easier in the long run.
Every person has different needs. Someone with stroke effects might need help on one side of their body. A person with Parkinson’s disease may struggle with tremors.
Meanwhile, someone with arthritis feels joint pain during gripping motions. Understanding these differences helps you provide better support.
A caregiver's guide to adaptive dining is a comprehensive approach that combines specialized equipment, environmental modifications, and assistance techniques to help people with disabilities eat independently and safely.
This method focuses on creating supportive dining environments, using proper feeding assistance techniques, and maintaining dignity while addressing challenges from conditions like stroke, Parkinson's disease, arthritis, and dementia.
This guide emphasizes assessment of individual needs, strategic meal preparation, family integration, and long-term planning to ensure successful mealtime experiences for both caregivers and care recipients.
ASSESSING INDIVIDUAL DINING NEEDS
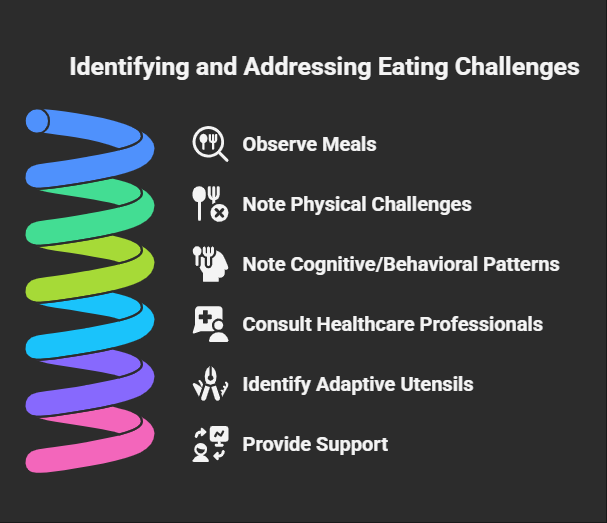
Before making changes, you need to understand current challenges. Start by watching several meals without helping.
Note what works well and what causes frustration. This observation period gives you valuable information.
Look for physical challenges first. Does your loved one have trouble holding utensils? Can they lift cups without spilling?
Do they struggle to cut food? These observations help you identify which adaptive utensils for poor grasp might be helpful.
Next, watch for cognitive or behavioral patterns. Some people eat too fast and risk choking. Others forget to eat entirely.
Some become frustrated and give up quickly. These patterns tell you about the kind of support needed.
Consider working with healthcare professionals during this assessment. Occupational therapists specialize in daily living activities like eating.
Speech-language pathologists help with swallowing concerns. Physical therapists can suggest better positioning for meals.
CREATING THE PERFECT DINING ENVIRONMENT
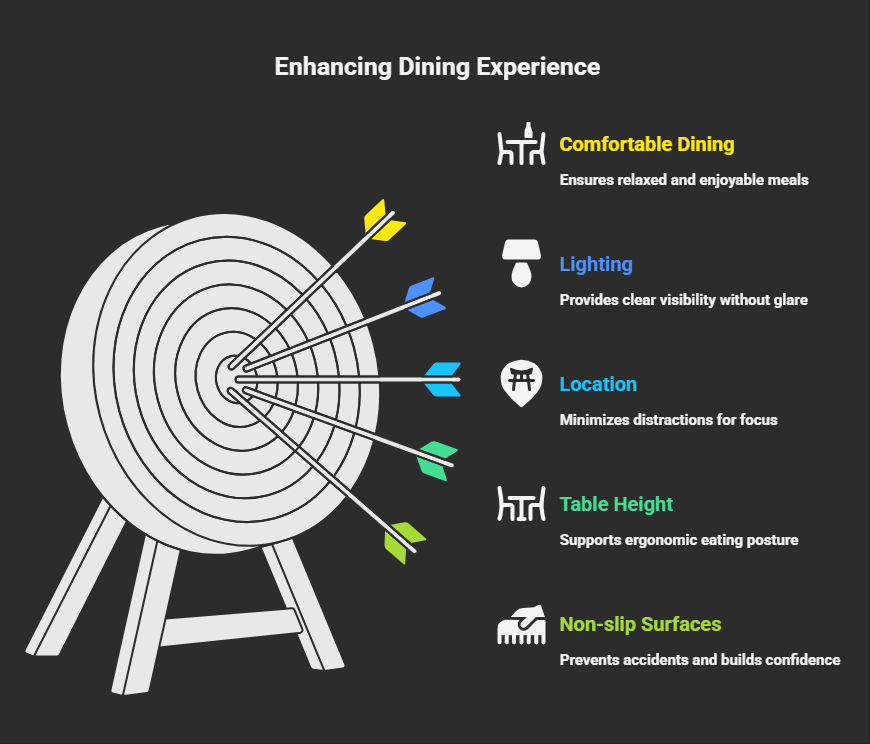
The right environment makes a huge difference in dining success. Start with lighting that’s bright enough to see food clearly.
Avoid harsh overhead lights that create shadows on plates. Instead, use soft lighting that reduces glare.
Choose a quiet location away from distractions. Turn off the television during meals. Put away phones and tablets. This helps your loved one focus on eating without competing stimulation.

The dining surface matters too. Use a table that’s the right height for comfortable eating. The person’s elbows should bend at about 90 degrees when holding utensils.
If the table is too high or low, add cushions or find a different chair.
Consider the temperature of the room. People with certain conditions feel cold more easily. A warm, comfortable environment encourages longer, more relaxed meals.
This is especially important for people who eat slowly due to their condition.
Non-slip surfaces help prevent accidents. Place rubber mats under plates and cups. This simple change reduces spills and gives your loved one more confidence while eating.
SMART MEAL PREPARATION STRATEGIES

Preparation work before meals makes everything easier. Cut food into smaller pieces ahead of time. This reduces the physical effort needed during eating.
It also prevents frustration when your loved one can’t manage cutting tasks.
Think about food temperature and texture. Many people with disabilities prefer foods that aren’t too hot or cold.
Extreme temperatures can be harder to manage safely. Similarly, consider textures that are easier to chew and swallow.
Arrange food on the plate in an organized way. Put meat in one area, vegetables in another, and starches in a third spot.
This organization helps people with vision problems or cognitive changes. It also makes the meal feel less overwhelming.
Use contrasting colors on plates. Light-colored foods show up better on dark plates. Dark foods are easier to see on light-colored dishes. This simple change helps people see their food more clearly.
FEEDING ASSISTANCE TECHNIQUES
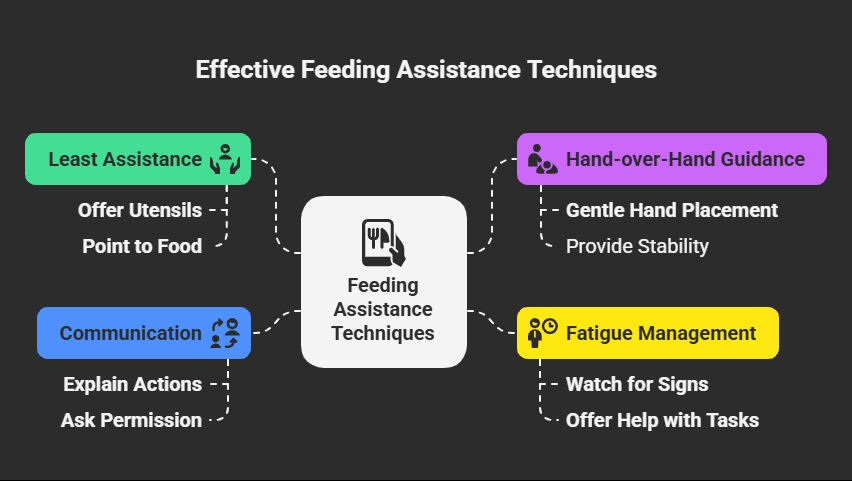
Knowing when and how to help takes practice. Start by offering the least amount of help possible. You might simply hand over a utensil or point to food on the plate.
Only increase assistance if the person clearly needs more help.
Hand-over-hand guidance works well for many people. Place your hand gently over theirs and guide the motion.
Let them do as much of the work as possible while you provide stability. This technique maintains their involvement in the process.
Watch for signs of fatigue during meals. Many people with disabilities tire quickly. When this happens, offer to help with more difficult tasks.
You might cut the remaining food or bring the utensils closer to their hand.
Communication during assistance is important. Explain what you’re doing and ask permission when possible. Say things like, “Can I help cut your meat?” or “Would you like me to move your cup closer?”
This maintains respect and dignity.
MANAGING COMPLEX CONDITIONS
Some people have multiple conditions that affect eating. For example, someone might have both stroke effects and dementia.
Others may deal with Parkinson’s disease along with arthritis. These combinations require flexible approaches.
When tremors are the main issue, weighted silverware for tremors can be very helpful. The extra weight provides stability and reduces shaking motions.
However, if arthritis is also present, the extra weight might cause joint pain. In these cases, you need to find a balance between stability and comfort.
People with progressive conditions need plans that change over time. What works today might not work in six months.
Keep in touch with healthcare providers about equipment changes. Document what works and what doesn’t to help with future decisions.
Behavioral challenges require patience and creativity. Some people become agitated during meals. Others may refuse certain foods or utensils.
Try different approaches until you find what works. Sometimes a change in routine or environment makes a big difference.
SUPPORTING INDEPENDENCE AND DIGNITY
Maintaining dignity during meals is crucial for emotional well-being. Always ask before helping with any task.
Give your loved one time to try things themselves before stepping in. Even if it takes longer, independence is worth protecting.
Adaptive plates for elderly users and others can promote self-feeding. Plates with raised edges help people scoop food more easily.
Divided plates keep different foods separate. These tools support independence while reducing frustration.
Encourage your loved one to participate in meal planning and preparation when possible. This involvement gives them control over their dining experience. It also provides mental stimulation and purpose.
Create positive associations with mealtime. Play soft music that they enjoy. Use their favorite dishes when possible.
Share pleasant conversation during meals. These elements make eating more enjoyable and less stressful.
FAMILY AND SOCIAL DINING
Including your loved one in family meals takes extra planning but provides important social benefits.
Other family members may need education about appropriate ways to help.
Teach children and adults how to offer assistance respectfully.
When eating out, call restaurants ahead of time. Ask about accessibility features and explain any special needs.
Many restaurants are happy to accommodate requests like pre-cutting food or providing eating utensils for the disabled.
Prepare a portable kit for dining away from home. Include necessary adaptive equipment, napkins, and cleanup supplies.
Having familiar tools available reduces anxiety and increases success in new environments.
Practice social dining skills at home first. This builds confidence for public outings. Start with short restaurant visits during less busy times.
Gradually increase the complexity of dining experiences as comfort levels improve.
TECHNOLOGY AND MODERN SOLUTIONS
Today’s technology offers new ways to support adaptive dining. Tablet timers can remind people when to take bites or sips.
This helps those who eat too quickly or forget to stay hydrated. Phone apps can track nutrition intake for caregivers who monitor dietary needs.
Video calling technology allows remote support during meals. Family members who live far away can provide encouragement during difficult mealtimes.
Healthcare providers can observe eating challenges through video calls and suggest improvements.
Smart home devices can provide voice reminders about mealtime routines. They can also play calming music or provide entertainment during longer meals.
However, keep technology simple to avoid overwhelming the person you’re caring for.
Some newer adaptive equipment includes built-in technology. Cups that light up when it’s time to drink help with hydration.
Plates that keep food warm automatically keep meals at safe temperatures. While these items cost more, they may provide valuable support for some people.
NUTRITIONAL MONITORING AND HEALTH
Keeping track of nutrition becomes more important when eating is challenging. Watch for signs of weight loss or dehydration.
These changes can happen gradually and may not be obvious day-to-day.
Work with dietitians when possible. They can suggest nutrition-dense foods that are easier to manage. They also help with meal planning that meets both nutritional and practical needs.
Monitor hydration carefully. Many people with eating challenges don’t drink enough fluids. Offer small amounts of liquid frequently throughout the day.
Use cups with straws or special lids if regular cups are difficult to manage.
Consider the timing of medications with meals. Some medicines work better with food. Others can affect appetite or taste. Understanding these interactions helps you plan better meal schedules.
CAREGIVER SELF-CARE AND SUPPORT
Caring for someone with eating challenges can be stressful. Meals may take much longer than usual. Progress can be slow or inconsistent. It’s normal to feel frustrated or worried sometimes.
Build a support network with other caregivers who understand similar challenges. Online groups and local support meetings provide valuable advice and emotional support. Don’t try to handle everything alone.
Take breaks when possible. Ask family members or friends to help with some meals. Even short breaks help prevent caregiver burnout.
Remember that taking care of yourself helps you provide better care for your loved one.
Continue learning about your loved one’s condition. New research often leads to better tools and techniques. Stay in touch with healthcare providers about new options that might help.
LONG-TERM PLANNING AND EQUIPMENT CHANGES
Conditions that affect eating often change over time. Equipment that works today may not be suitable in the future. Plan for these changes by staying informed about progression patterns.
Keep records of what works and what doesn’t. This information helps healthcare providers make better recommendations. It also helps you make decisions about new equipment purchases.
Consider the cost of adaptive equipment over time. Some items may need replacement as conditions progress.
Others might be used for many years. Insurance may cover some costs, so check with providers about coverage options.
Think about care transitions that might occur. If your loved one needs to move to assisted living or needs additional care, their dining equipment should move with them.
Make sure care providers understand how to use any special tools.
CONCLUSION
Creating successful adaptive dining experiences requires patience, creativity, and flexibility. It’s about much more than having the right equipment.
The environment, techniques, and emotional support you provide all contribute to positive outcomes.
Remember that every person’s needs are unique. What works for one person may not work for another.
Stay observant and willing to make changes as needed. Small adjustments often make big differences in dining success.
Most importantly, focus on maintaining dignity and independence whenever possible. Meals should be enjoyable social experiences, not just about getting enough nutrition.
With the right approach, adaptive dining can preserve quality of life and family connections.
Your role as a caregiver is challenging but incredibly important. The support and understanding you provide help your loved one maintain independence and enjoy mealtime experiences.
Take pride in the difference you make in their daily life.